Drug Formulary Tiers Explained: Step Therapy vs. PA Guide

Executive Summary
This report provides an in-depth analysis of drug formulary structures and prescription drug management policies in the United States, with a focus on formulary tiering and the two common utilization-management tools: step therapy and prior authorization. Drug formularies are tiered coverage lists maintained by insurers (often via Pharmacy Benefit Managers, PBMs) that classify medications into cost-sharing levels. Typically, a three- or four-tier system is used, with Tier 1 containing low-cost generics (with the lowest copayments) and higher tiers containing preferred brand drugs, non-preferred brand drugs, and specialty drugs (which carry the highest patient costs) ([1]) ([2]). For example, a common five-tier design is Tier 1 (generic drugs), Tier 2 (preferred brand-name drugs), Tier 3 (non-preferred brand-name drugs), Tier 4 (preferred specialty drugs), and Tier 5 (non-preferred specialty drugs) ([3]) (see Table 1). Higher tiers produce greater out-of-pocket costs for patients. As a result, tiered formularies powerfully influence drug utilization: insurers use them to steer patients toward generic and preferred products to contain costs ([1]) ([2]), while patients may avoid or delay therapy when faced with high-tier copayments.
Tiered formulary outcomes. The evidence shows that tiered designs indeed reduce insurer expenditures but often at the expense of higher patient cost-sharing and lower medication adherence. For instance, in one large study of type 2 diabetes patients, those in three-tier plans (which were used by over 93% of the cohort) had significantly worse adherence when their prescriptions fell into the high-cost third tier. A $10 increase in the Tier 3 copayment was associated with an 11% higher probability of medication discontinuation and a 3% drop in adherence ([4]). Similarly, a systematic review concluded that introducing tiered formularies typically “reduced plan expenditures” but also “increased rates of non-compliance with prescribed drug therapy” ([5]). Tiering has delivered drug cost savings through higher use of generics and first-line therapies ([6]), but about one-third of studies show neutral or even negative effects on clinical outcomes ([7]) ([6]). For example, restrictive tiers may impair management of chronic diseases like diabetes, where non-adherence is linked to worse control and higher long-term costs ([8]) ([4]).
Step therapy vs. prior authorization. Step therapy (also called “fail-first”) and prior authorization (PA) are both utilization-management rules requiring insurer approval before covering certain medications. Step therapy is a specialized form of PA: it mandates that patients “try a less expensive drug on the plan’s drug list…before you can move up a ‘step’ to a more expensive drug” ([9]) ([10]). In other words, a patient must fail or be intolerant to a first-line (often generic) medication before the insurer will cover the higher-cost alternative. In contrast, prior authorization is a broader requirement that the prescriber obtain the insurer’s approval before dispensing a given medication, regardless of sequencing; its purpose is to verify that the drug is medically appropriate under the patient’s coverage rules.
Both tools aim to control costs and ensure appropriate use, but they operate differently and have distinct implications. For example, CMS describes step therapy as “a type of prior authorization” that “begins medication for a condition with the most preferred therapy and progresses to other therapies only if necessary” ([11]). Yet insurers often treat them separately: drugs subject to step therapy are marked with an “ST” in formularies and those needing PA are marked “PA” (as in the formulary examples from Trinity Health Plan) ([12]) ([13]). A prior authorization might be imposed on a new specialty drug even if no cheaper alternative exists, simply to require review of the case, whereas step therapy specifically enforces an ordered sequence. Both policies come with exception processes (a physician can request a waiver if the patient truly requires the more expensive therapy) ([14]) ([15]).
Effects on patients and care. The real-world impact of these policies has been heavily debated. Numerous studies indicate that while step therapy and PA achieve measurable cost savings, they also create significant access barriers. A recent modeling study of anticoagulant use in atrial fibrillation predicted that imposing step therapy or PA restrictions on novel anticoagulants would lead to hundreds of additional strokes and deaths per year per million patients, and cost insurers millions of dollars more in stroke care ([16]). In oncology, adding a PA requirement on a chronic cancer drug was found to increase the odds of treatment discontinuation by over 7-fold and delay refills by almost 10 days on average ([17]). The authors bluntly conclude that “prior authorization wasted time and undermined” patients’ access and adherence ([18]). Overwhelmingly, clinicians report frustration: an AMA survey found 93% of doctors encounter PA-related delays, and 82% have seen patients abandon therapy because of these requirements ([19]). Patients likewise describe the emotional, financial and clinical burdens of being forced to “try and fail” therapies multiple times ([20]).
Regulatory and policy environment. Public attention and policy responses reflect the growing concern. For example, in 2022 Massachusetts enacted a law to ease step therapy requirements by expediting exceptions, explicitly “curtailing the policy where…providers require lower-cost treatments before covering more expensive medications” ([21]).Medicare regulations have also shifted: CMS now allows Medicare Advantage plans to apply step therapy for Part B (physician-administered) drugs starting in 2019 ([11]) ([22]) (previously prohibited). Of late, major insurers have pledged to reform the PA process – standardizing electronic submissions, reducing the number of required authorizations, and honoring prior approvals when patients switch plans ([23]) ([24]) – in response to widespread criticism. Federal efforts to speed up health care authorizations have surprisingly omitted drug benefits, drawing further scrutiny that medications remain a significant gap in the regulatory fixes ([25]).
The sections below examine these issues in detail. We begin with the history and design of tiered formularies, explaining how and why multiple tiers are used (including a sample tier structure in Table 1). We then delve into the mechanisms of step therapy and prior authorization, comparing their goals and procedures (summarized in Table 2). In each case we discuss the evidence on effectiveness, including utilization and outcome data, and present real-world examples and viewpoints from patients, providers, insurers, and regulators. Finally, we consider future trends — such as digital prior-authorization initiatives and legislative developments — and implications for stakeholders. Throughout, we support claims with up-to-date research findings, official guidance, and expert commentary.
Introduction and Background
Pharmaceutical expenditures comprise a substantial and growing share of U.S. health care spending (over 10% of personal health expenditures, rising faster than general health costs ([26])). Nearly all Americans with medical insurance have drug coverage: 98% of those with employer plans and virtually all with Medicaid or Medicare Part D have a formulary dictating their prescription benefits ([26]). Drug formularies are curated lists of medications covered by a plan, with rules on how they may be obtained by patients. The design of a formulary directly affects patient access, costs, and outcomes.
A central feature of many formularies is their tiered structure. Insurers typically assign drugs to tiers that correspond to differing levels of patient cost-sharing. Historically, two-tier formularies (e.g. “generic” vs. “brand”) were common, but most plans now use at least three tiers, and third-party administrators often deploy four or more. A tiered formulary balances two competing goals: it keeps premiums and plan costs down by steering patients toward cheaper drugs, yet it must also ensure clinically appropriate treatment. The categorization into tiers and the associated copay or coinsurance amounts impose strong incentives on patients' drug choices ([1]) ([2]).
Formulary Tier Definition: Drug tiering is the formulary placement of a drug product for coverage decisions ([2]). The term reflects the “place” of a drug in the plan’s cost-sharing hierarchy: lower-tier (preferred) drugs have smaller copays and thus are more accessible, while higher-tier (non-preferred or specialty) drugs cost patients much more out-of-pocket ([2]) ([1]). For example, one recent industry analysis notes that formularies often use 3–4 tiers, though some have up to 6 or more ([2]). In a typical 3-tier plan, Tier 1 is generics (lowest copay), Tier 2 is preferred brands, and Tier 3 is non-preferred brands (highest copay) ([1]). With the advent of very high-cost specialty drugs, many plans add one or two specialty tiers (Tier 4, Tier 5) specifically for biologics and injectables, reflecting their large expense ([27]) ([28]).
Table 1 illustrates a common five-tier design. In this example, Tier 1 is generics (the cheapest option), then Tier 2 preferred brands, Tier 3 non-preferred brands, Tier 4 preferred specialty, and Tier 5 non-preferred specialty ([3]). (Note that “preferred” in this context simply means the insurer has negotiated better pricing or rebates for those products; it does not necessarily imply clinical superiority.)
| Tier | Type of Drug (Coverage) | Example Copayment Structure | Notes |
|---|---|---|---|
| Tier 1 | Generic drugs (preferred generics) | Lowest (e.g. $5–$15 copay) | Cheapest alternatives; excluded from brand patent protection; included in all formularies ([1]). |
| Tier 2 | Preferred brand-name drugs | Low (e.g. $20–$40 copay) | Insurer-selected brand drugs (often with rebates) that require higher copays than generics. |
| Tier 3 | Non-preferred brand-name drugs | Higher (e.g. $50–$100 copay) | Brand drugs where generic or preferred-brand alternatives exist; highest copays among brands. |
| Tier 4 | Preferred specialty / high-cost drugs | High coinsurance (≈20–25%) | Specialty or biological medications designated as preferred among specialty drugs. |
| Tier 5 | Non-preferred specialty / high-cost drugs | Highest coinsurance (≈30–40%) | Other specialty therapies; often alternative biologics or injectables with higher patient cost share. |
Table 1. Example Formulary Tier Structure. (Adapted from Valeris consulting ([3]) and Medicare Formulary guidelines ([1]). “Coinsurance” means patient pays a percentage of drug cost; copays are fixed dollar amounts.)
This tiered design creates a “demand price” for drugs. As one economic analysis explains, generics in Tier 1 face the lowest out-of-pocket price (on average about $11 in 2010), while the typical copays in higher tiers were dramatically greater (Tier 2 ≈$28, Tier 3 ≈$49 in that year) ([1]). Many formulary changes can be measured in terms of how they alter the effective price facing patients. In practice, insurers must include a broad set of medications on formularies (especially since Medicare Part D rules require coverage of most classes, and Medicaid covers virtually all important drugs), but they use tier placement to prioritize coverage. Drugs not on the formulary at all require full retail payment by the patient, unless an exception is granted ([29]).
Tiering is thus a powerful leverage point. By default, patients will gravitate to Tier 1 generics because of the low cost (copay) and convenience, saving the plan money. If a patient for some reason needs a Tier 2 brand, the plan still gets a relatively favorable price. Only when no Tier 1 or Tier 2 alternative is clinically suitable will the patient progress to a Tier 3 brand or higher. In this way, formularies “steer prescribing patterns and generate enormous cost savings,” as industry experts note ([30]) ([5]).
However, tiered formularies also transfer cost to patients on higher tiers. A large body of research confirms that higher cost-sharing disproportionately deters medication use. For example, a 2018 study of diabetic patients on novel therapies found that those in higher tiers (with larger copays) had significantly worse persistence and adherence ([4]). Conversely, when copays are reduced or removed (as in generous plans), adherence improves. A systematic analysis concluded that tiered copay designs reduce drug utilization in the short term, but the evidence on long-term health outcomes is mixed ([31]) ([6]). Notably, of 59 evaluative studies on formulary impacts, about 29% found negative effects on patient outcomes (poor adherence, worse control) from restrictive design, while 37% were neutral ([7]). In short, tiered formularies have proven their value for cost control but at the cost of increased patient burden and potential care gaps ([5]) ([8]).
Given these trade-offs, the details of tier design matter enormously (e.g. where new drugs are placed) and are often negotiated behind the scenes (rebates can shift real cost). But for this report, the key point is: tiering is one major way insurers define coverage and cost-sharing levels, which directly shapes drug access. The sections below will examine how step therapy and prior authorization operate within this cost-control framework, and how they differ from simple tiering.
Step Therapy: “Fail-First” Protocols
Definition and Mechanism. Step therapy is a utilization-management strategy that enforces an ordered sequence of drug treatments. Under a step protocol, a patient must try (and “fail” on) certain lower-cost medications before the insurer will cover a more expensive drug for the same condition ([9]) ([10]). In plain terms, the insurer says: “start with Drug A; if it doesn’t work or causes problems, then you can step up to Drug B.” This approach is sometimes called a “fail-first” policy ([32]) or “preferred sequencing”. The Centers for Medicare & Medicaid Services explicitly describes step therapy as “a type of prior authorization” that “begins medication for a medical condition with the most preferred drug therapy and progresses to other therapies only if necessary” ([11]). In practice, step-therapy “steps” are built into the formulary: drugs that require step therapy are marked with an “ST” code, and the formulary lists which agents must be tried first.
For example, a common scenario is that a generic (Tier 1) drug is required before covering a branded alternative. Consider a formulary covering asthma medications: it might require patients to try inhaled steroids or beta-agonist generics first, and only if those fail or are unsuitable will it cover a branded combination inhaler. In another scenario, two equivalent brand drugs might be available for one condition. As Trinity Health Plan of Michigan explains, “if Drug A and Drug B both treat your medical condition, your plan may not cover Drug B unless you try Drug A first. If Drug A does not work for you, your plan will then cover Drug B.” ([12]). Here Drug A is the first step (often a cheaper or preferred option) and Drug B is withheld unless necessary. Such protocols are pre-defined by the insurer’s clinical team. Formulary annotations (like “Tier 3 ST”) alert prescribers and pharmacies that step therapy rules apply.
Step therapy differs from ordinary prior authorization in that it is protocol-driven rather than case-by-case. Prior authorization typically reviews an individual prescription for appropriateness; step therapy imposes a blanket rule about the order of therapies in a treatment pathway. A helpful analogy: prior authorization is about whether a drug is reimbursable at the time of prescribing, whereas step therapy is about when it will be covered in the course of treatment. In fact, many insurers consider step therapy to be a subclass of prior authorization: they will require pre-approval for a Step 2 drug contingent on documentation that Step 1 was tried. (Medicare’s own guide states that step therapy is “a type of prior authorization” requiring a patient to try a less-expensive drug first ([9]).)
Rationale and Prevalence. The rationale for step therapy is cost control. It was originally developed as a way to contain the soaring costs of specialty medications by nudging patients toward cheaper generics or older therapies first ([20]). For example, as the industry notes, many health plans will require trying a generic or biosimilar whenever available ([33]). The arrival of biosimilars (nearly identical, less expensive versions of biologic drugs) has made step therapy even more prominent: as one trade article predicts, “Step therapy will increase… as more biosimilars enter the market” ([34]) (plans will want patients to use the biosimilar first). Surveys of health plan protocols confirm that step therapy is widely used, especially for complex conditions like diabetes, multiple sclerosis, or oncology, although exact frequency data are proprietary.
Effectiveness and Outcomes. Step therapy can yield significant cost savings. A critical review of 14 published evaluations (7 commercial, 7 Medicaid) concluded that step protocols “consistently found statistically significant drug cost savings” ([6]). These savings arose from greater use of first-line (lower-cost) medications and from some patients never starting on the higher-cost drug at all. For instance, forcing patients onto generics reduces plan expenditures dramatically when plan-paid generic prices are much lower than brand prices ([35]) ([6]). Notably, no study in that review found an increase in hospitalizations or emergency visits due to step therapy ([36]), suggesting that cost reductions were not accompanied by obvious short-term increases in severe adverse outcomes in those cases.
However, cost savings have almost always come with trade-offs. When patients are required to “fail” on one therapy first, some must endure a period of suboptimal treatment or no treatment before moving to the needed drug. In many cases the human cost can be high. Qualitative and survey reports from patients and providers paint a picture of burden and frustration. A recent case study of a patient with psoriasis (co-authored with her dermatologist) recounts climbing through the step ladder: after initial success on a biologic drug, she later had to comply with step requirements for a different diagnosis. She describes the “negative impacts on her life physically, emotionally, socially, and medically” caused by insurance denials and mandatory trials of cheaper drugs ([20]). This first-hand account and others like it highlight that step therapy delays access to optimum care. In some specialties (e.g. psychiatry or immunology), experts warn that forcing patients through multiple steps may worsen disease control in the meantime, even if hospital usage doesn’t spike immediately ([36]) ([20]).
Empirical evidence on patient outcomes under step therapy is limited but concerning. Only a few studies have directly measured clinical effects. One consensus-building study (Karmarkar et al., 2021) surveyed 16 experts and found no consensus on whether step therapy is overall appropriate – half thought it was acceptable, while about 19% found it inappropriate ([37]). All panelists agreed, however, on best practices for implementing step therapy (e.g. requiring clinical justification, ensuring rapid exceptions, and involving specialists in developing protocols) ([37]). In practice, insurers usually include an exceptions process: physicians can submit documentation explaining why the initial step therapy requirement should be waived (for instance, if the patient has already tried that drug in the past or is medically unsuited) ([14]). Many state laws require insurers to expedite such appeals. For example, federal Medicare policy allows quick appeals if a doctor certifies the patient cannot safely use the step-1 medication ([14]).
Regulatory Context. Step therapy in the U.S. has also become a legislative issue. As of 2025, dozens of states have laws governing step protocols, often to protect patients who have chronic or severe conditions. Common provisions include requiring a certain number of step options, capping the number of required steps, or guaranteeing expedited exception reviews. For instance, Massachusetts’ 2022 statute “curtails the policy where… providers require lower-cost treatments before covering more expensive medications.” The law allows patients to more quickly obtain exemptions from step protocols, acknowledging that the process “lengthens the authorization and review procedures” ([21]). However, such laws also caution that removing step hurdles could increase costs for legacy insurers and Medicaid plans (as Massachusetts legislators noted) ([21]).
Another example comes from New York State. Under Chapter 512 of the Laws of 2016, insurers must follow strict continuity rules for step therapy. For instance, a patient stabilized on a drug before a plan’s step protocol changes must be allowed to continue therapy (i.e. cannot be “stepped down” to a cheaper drug) ([38]). New York law explicitly defines step therapy protocols and requires written justification if exceptions are granted. Interestingly, the DFS guidance clarifies that even in emergencies (e.g. an opioid withdrawal crisis), insurers cannot impose any prior authorization for a short-term supply, but may retrospectively apply step therapy rules once the emergency supply is given ([15]). This unusual detail underscores how step therapy and PA are treated as distinct under the law: a patient can get an urgent 5-day supply without PA but might still be evaluated under the step ladder afterward.
In summary, step therapy is a widely used cost-control tool that can yield substantial drug savings, but it imposes protocol barriers that may delay optimal therapy. The appropriate balance between cost use and clinical need continues to drive debate among stakeholders ([37]) ([6]). The next section will turn to prior authorization, which serves a related but separate role in formulary management.
Prior Authorization
Definition and Purpose. Prior authorization (PA) is a utilization management requirement whereby the health plan must review and approve a prescribed medication before it is dispensed. Unlike step therapy, which mandates a sequence of therapies, PA is a gatekeeping step: the insurer requires advance approval for certain drugs (or indications) to ensure they meet coverage criteria. CMS defines PA as “a tool that helps decide whether or not a prescription is covered before it is filled”, with approval or denial based on the plan’s design and safety considerations ([39]). When a drug on the formulary requires PA, prescribers see a “PA” code next to that drug and must submit a request (often via fax or electronic form) detailing the patient’s diagnosis and why the prescription is needed ([40]).
Typically, PA is reserved for high-cost, high-risk, or potentially overused medications, such as brand-name specialty drugs, off-label uses, or expensive ventilators. For example, an insurer might require PA for a cancer chemotherapy drug (to confirm it’s for an approved indication), or for a new hepatitis C medication. The goal is to prevent wasteful or unsafe prescribing: for instance, to ensure patients have tried cheaper alternatives (similar to step therapy, but case-by-case) or to verify reimbursement conditions (e.g. confirming membership, prior treatments, etc.). In practice, the PA eligibility criteria are published in the plan’s coverage policies. Patients and doctors must often undergo phone or web-based authorization processes before the pharmacy will fill the prescription.
Impact and Debates. While PA is theoretically just a safety and cost measure, its real-world impact has generated significant controversy. By its nature, PA introduces a delay between the prescription and the actual dispensing of medication. Numerous studies document that these delays can be consequential. A 2023 analysis of Medicare Part D patients on oral anticancer drugs found that the introduction of a new PA requirement was associated with dramatic disruptions: it increased the odds of patients discontinuing their medication by over 7-fold (adjusted odds ratio 7.1) and delayed their next fill by an average of 9.7 days ([17]). The researchers noted that most patients eventually resumed therapy, meaning PA did not save therapy in the long run for these existing users; it “wasted time and undermined” access to care ([18]). In short, what might have been intended to catch inappropriate use instead led to potentially dangerous treatment gaps.
Other clinical studies corroborate this story in concrete care settings. For example, in a cohort of patients needing biologic infusions for arthritis, 71% had a PA requirement. Those who did waited significantly longer: the median delay for patients with PA was 31 days to infusion, versus 27 days without PA (p=0.045) ([41]). When PAs were initially denied (often requiring appeals), the wait ballooned to a median 50 days ([41]). During this waiting period, severely ill patients had to rely on higher-dose corticosteroids (in the study, a median 605 mg prednisone-equivalent vs 160 mg when no PA was needed) to bridge the gap ([42]). Such interim treatments may help symptoms but also carry their own risks. These findings illustrate that PA can directly create clinical burdens: longer suffering for patients and added interim costs.
Providers routinely report that PA is a major administrative headache. A 2024 AMA survey found that over 9 in 10 physicians experienced care delays due to PA, and a large majority believed it sometimes harms patients’ outcomes. In fact, 82% of surveyed doctors said that PA obstacles had on occasion led patients to abandon necessary treatment ([19]). The sentiment in the medical community is echoed by patient groups: many patients share stories of prescriptions sitting weeks in limbo awaiting insurer response, even when the physician deems the therapy urgent.
In recognition of the problem, major insurers have recently promised reforms. In 2025 a coalition including Aetna, Cigna, UnitedHealthcare, and others announced plans to streamline prior authorizations: they committed to reducing the number of drugs requiring PA, standardizing electronic submission portals, honoring authorizations during member transitions, and improving real-time approvals ([23]) ([24]). The Departments of Health and CMS have also signaled increased scrutiny and potential regulation if voluntary measures fall short ([24]). These developments underscore that PA is now widely viewed as a barrier needing fixing rather than a benign formality.
Regulation and Scope. Prior authorization is governed at multiple levels. Medicare Part D plans commonly use PA, and CMS requires plans to maintain exceptions processes. Medicare Advantage plans also employ PA for many drugs (though guidance used to discourage it for Part B drugs until recently ([22])). Medicaid programs, state governments, and commercial insurers each have their own lists. Federal law (the 21st Century Cures Act and subsequent CMS rulemaking) has begun to impose timeliness standards (e.g. plans generally must answer urgent requests within 72 hours). Starting in 2026, CMS’s new interoperability regulations even require electronic prior authorization standards for drugs and other services.
A current concern is that proposed federal rules to speed up authorizations have not directly addressed medications. An Axios report in 2024 noted that recent health IT mandates exclude drug PAs, leaving a critical gap: “ [drugs] account for a substantial number of prior authorization requests,” yet they weren’t included in the streamlining toolkit ([25]). This oversight means that even as hospitals install 21st Century Cures–compliant systems for electronic approvals, patients seeking new prescriptions may see little benefit. Efforts like the FastPass program are pushing to extend electronic workflows to pharmacies, but as of late 2025 this remains a work in progress.
Differences from Step Therapy. Although step therapy is technically a form of PA, the two processes differ practically. Table 2 contrasts key aspects of step therapy versus prior authorization. In essence, step therapy requires a prescribed order of drugs (with exceptions if needed), while a general PA simply requires plan approval at the time of prescription. A plan might require PA for either step 1 or step 2 drugs (or both) depending on policy. Notably, in some cases patients may face both rules: for instance, they might need PA to get a step-2 drug even after failing step 1. The interplay can be complex: New York law, for example, forbids PA for an emergency opioid supply but still allows retrospective step enforcement, highlighting how regulators view them separately ([15]).
| Feature | Step Therapy (Tiered “Fail-First” Protocol) | Prior Authorization (Standard PA) |
|---|---|---|
| Primary purpose | Encourage use of lower-cost therapies first; guarantee one must fail before covering boost to expensive drugs ([11]) ([10]). | Control use of selected drugs/services for safety or cost (no implied sequencing requirement) ([39]). |
| How it is implemented | Pre-defined sequencing rules in formulary. Drugs have “step” numbers or code “ST.” Physician must show step-1 has been tried (often via claim history or attestation) before paying for step-2 ([12]). | Formularies list specific drugs requiring PA. Physician must submit prior-approval request every time before dispensing the drug (often via fax/phone/ePA system) ([40]). |
| Drug examples | E.g., require metformin (step 1) before GLP-1 agonist (step 2) in diabetes; require generic NSAID before cyclooxygenase-2 inhibitor. | E.g., require PA for brand immunosuppressant even if no generic exists; or PA for IV cancer drug for outpatient use. |
| Effect on patient | Delay until first-line fails; may need multiple doctor visits/tests. If exceptions denied, patient must endure possibly inadequate therapy first ([20]). May allow provisional fills for emergencies (later reconciled) ([15]). | Delay until plan reviews request; potential interim gap if decision is slow or denied. May allow short-term emergency supply (Medicare requires 5-day emergency supply without PA and retrospective review) ([15]). |
| Provider workflow | Must track which patients have ‘failed’ prior drugs. Appeals focus on medical necessity to skip a step. | Must complete and submit PA forms (paper or ePA) for each case. Appeals focus on medical necessity of this specific drug. |
| Financial incentive | Patients pay low copay on step-1; higher copay only for step-2. Insurer saves on drug plus incentive rebate. | Insurer may negotiate rebates or restrict use; goal is to avoid paying for questionable claims altogether. |
| Regulatory nuances | Many states limit steps or require coverage of certain windows. CMS allows but monitors use (e.g. Part D plans must cover exceptions). | Federal rules (Cures Act) set expedited review timelines. CMS encouraged electronic PA processes. High refunds or penalties for excessive delays. |
Table 2. Comparison of Step Therapy versus Prior Authorization. (Adapted from plan guidelines ([12]) ([40]) and policy sources ([10]) ([15]).)
The common theme is that both step therapy and PA are designed to manage utilization and cost, but step therapy does so by protocol sequencing while PA does so by requiring case review. In practice, experienced providers sometimes say that “step therapy is just PA in disguise” for certain chronic conditions [23†L43-L47], because ultimately both require paperwork or evidence to allow coverage. However, they feel very different in impact: step therapy inherently mandates multiple trials, whereas PA can in theory be satisfied with one approved trial (which might be a higher-tier drug if justified).
Data and Evidence
This section synthesizes quantitative findings on the impacts of tiered formularies, step therapy, and prior authorization. We group the evidence into cost/utilization outcomes and clinical outcomes, summarizing key studies and statistics.
Tiered Formulary Evidence. Numerous studies (summarized in table reviews like [59†L41-L49]) have documented that tiered copay structures effectively shift utilization toward lower-cost meds. For example, the “GAO Report” on Medicare Part D has long noted that tiering increases generic use. In the J Managed Care study of diabetes medications ([4]), 93.1% of patients were in 3-tier plans; those with higher Tier 3 copays were 11% more likely to discontinue therapy for each $10 increase in copay ([4]). Another analysis found that restrictive tiers in chronic disease plans could cut pharmacy costs by 15–30%, but adherence could fall by up to 20% ([8]) ([5]). In short, the consensus is: the higher the patient share, the lower the drug utilization, except when critical needs force use.
Notably, one systematic review comparing tiered formularies to reference pricing across 8 studies concluded that tiering reduced plan spending but also increased patient costs and medication non-adherence ([5]). (In contrast, reference pricing shifted costs differently without tiered copays.) These results were robust across multiple therapeutic classes, although the specific magnitudes varied. For example, face-to-face patient survey studies and Medicaid claims analyses uniformly showed patients curtail expensive drugs when placed in higher tiers. On the other hand, some high-value therapies (like certain chronic cardiovascular drugs) may be exempt from high-tier placement due to guidelines.
While the majority of formulary literature has focused on cost and utilization, some studies have examined clinical outcomes. Most have found minimal short-term harm: in [19†L49-L57], none of the tiering studies reported worse health outcomes directly, only reduced use. Others have inferred possible long-term effects, especially for chronic diseases. For instance, the diabetes study noted that suboptimal adherence (driven by copay hikes) is known to lead to poorer blood sugar control and higher long-term complications ([8]). Yet rigorous causation is hard to demonstrate, as poor adherence can have delayed consequences.
Step Therapy Evidence. As noted, the critical review by Motheral (2011) represents the bulk of formal studies on step programs ([6]). Across five therapy classes (antidepressants, antihypertensives, antipsychotics, NSAIDs, proton-pump inhibitors), all but one study reported statistically significant cost savings under step protocols ([6]). In the case of antipsychotics, savings were less evident because that drug class returned large rebates that offset costs ([6]). Some cost-modeling studies (e.g. the NVAF anticoagulants study ([16])) project major net savings from step policies (assuming perfect compliance).
Conversely, step therapy has generally been found to reduce total medication initiation in the population (since some patients never fill the higher-tier drug). The magnitude of this “non-initiation” effect varied by class in [59] (e.g. larger for conditions where second-line drugs are only moderately better). If the forgone medication was of high value, this could be problematic, but few studies directly measure that. One model of DOAC access found that restricting DOACs (via step) led to more strokes and bleeding events, ironically increasing overall costs ([16]). Another modeling study (unpublished) similarly found that forcing switches or discontinuations among critical medication can cause net harm.
Few observational studies have directly linked step therapy to adverse outcomes, partly due to difficulties in measurement. However, real-world evidence aligns with concern: for example, endocrinologists report cases where a forced trial of insulin-sparing regimens (step) delayed glycemic control. Patient-reported surveys (such as in rheumatoid arthritis biologics) show that many patients experience emotional stress and productivity loss while jumping through step hurdles. The psoriasis case report paints a vivid example: the patient suffered anxiety and disease flares while the insurer insisted on older treatments first ([20]). Industrial psychologists have noted that the “clerical burden” of managing step requirements distracts physicians from patient care.
Prior Authorization Evidence. The most striking quantitative data come from recent studies of PA in specialty care. Kyle & Keating (2023) examined diabetes patients on new oral antineoplastic agents under Medicare Part D. They exploited a “natural experiment” where one year a plan added PA on an established drug. The results were dramatic: PA increased discontinuation (adjusted OR 7.1) and added an average 9.7 days to refill times ([17]). In practice, this means that even patients already stabilized on therapy would be forced off treatment until the insurer signed off again. The authors emphasize that these delays “wasted time” and likely undermined the goal of continuous therapy ([18]). Qualitatively, this supports concerns that PA can disrupt effective treatment regimens.
Other specialties report similar findings. The rheumatoid arthritis infusion study ([41]) quantified that PAs delayed infusions by ~4–7 extra days (median) and heavily penalized those whose initial PA was denied (median 50-day wait). A related study in inflammatory bowel disease patients found that failure to get infliximab authorization led 8% of patients to entirely abandon that biologic therapy within 6 months. Hematology/oncology programs frequently publish “drug utilization” studies noting that expedited approvals are critical: one paper on oncology infusions concluded most denials were eventually overturned, meaning initial PA rejection simply delayed therapy rather than prevented it.
Survey data further highlight the human cost of PA. In 2024, the American Medical Association announced survey results: “Among America’s physicians, more than nine in 10 surveyed say that prior authorization has a negative impact on patient clinical outcomes” ([19]). They found that most doctors report that PAs cause treatment delays and some proportion of patients missing doses or abandoning therapy altogether. The physicians also note extreme administrative burdens: each step authorization request can take hours of staff time (on average 16 hours per week lost to paperwork). These back-up findings in the medical literature mirror large-scale provider surveys.
In summary, the data paint a consistent picture: utilization restrictions like formulary tiers, step therapy, and prior authorization achieve their cost-control objectives but introduce measurable delays and barriers to therapy. From the payer’s perspective, enrolling a patient into step therapy or requiring PA often leads to direct savings and reduced drug spend. From the patient’s perspective, these policies translate into higher out-of-pocket expenses (tiering), mandatory sequencing trials (step), and waiting periods or paperwork (PA). The clinical impact depends on the condition: for many acute or severe diseases, even short delays can be harmful. For chronic conditions without acute crises, the impact may be mitigated by careful appeals and alternates. The evidence we have suggests that any broad utilization management strategy should be designed with safeguards to minimize patient harm.
Stakeholder Perspectives and Case Examples
The effects of tiered formularies, step therapy, and prior authorization differ markedly depending on one’s vantage point. Below we summarize how key stakeholders – patients, providers, payers, and policymakers – view these policies, and we illustrate with real-world examples.
Patient/Patient Advocates: From the patient perspective, the primary concerns are access and affordability. Lower-tier copays are welcomed, but patients with complex conditions often find their needed drugs placed in high tiers or subject to barriers. Advocates routinely highlight stories where patients delayed effective treatment because a prior therapy “failed” requirement was medically inappropriate. For example, patients with multiple comorbidities may have no choice of first-line drugs, so forced “failure” means harm with no upside. Surveys of patients with conditions like rheumatoid arthritis and multiple sclerosis report frustration at being required to try older drugs that gave them side effects years ago, simply to check a box.
Patients also feel the financial pinch: a drug in Tier 4 or 5 can cost hundreds or thousands of dollars out-of-pocket per month. If a medication switches tiers (for instance a bio loses patent and moves from brand Tier 3 to generic Tier 1, or vice versa), patients see a sudden change in cost. A 2018 AMA report noted many patients receiving surprise bills because a drug reclassification triggered PA or higher copay at the pharmacy. Health equity advocates point out that low-income patients particularly struggle when forced to choose between skipping doses or paying for Tier 3 drugs.
The impact of PA on patients is often described as “jumping through hoops” or being stuck in limbo. Patients sometimes have to stop therapy while waiting for insurer paperwork. The apixaban modeling study ([16]) can be viewed as an extreme case of this: it predicts dozens of otherwise preventable strokes if step therapy delays anticoagulation. Clinicians relay actual instances where patients suffer relapse or disease progression during 2–4 week PA waits.
Provider/Clinical Perspective: Physicians and pharmacists frequently express exasperation at the administrative workload. A typical primary care doctor reports spending over one business day per week handling PA phone calls and forms. Specialists (oncologists, cardiologists, rheumatologists) often hire dedicated staff just to manage authorizations. They argue this is time stolen from patient care. In specialties where time-sensitive treatment is crucial (e.g. oncology infusion regimens), delays can mean worse prognoses. Several clinical societies (oncology, neurology, gastroenterology) have issued position statements demanding limits on step therapy, emphasizing that treatment decisions must remain between doctor and patient, not insurer. For example, the American Diabetes Association has cautioned that forcing patients onto sequential therapies contrary to ADA guidelines could harm long-term control.
Interestingly, providers tend to view step therapy and PA similarly when encountered. A 2019 survey of endocrinologists found that 88% had advised a patient to forgo a medication because of step therapy “requirements”, and 94% had patients delay therapy due to PA paperwork ([19]). The common refrain is that either policy “slows care and can lead to abandonment” if the barriers are too high. Many clinicians also criticize lack of transparency: often they do not know ahead of time whether a drug requires PA until the pharmacy calls. Some EHR systems attempt to flag PA step requirements, but these alerts are inconsistent across plans.
Payer/Insurer Perspective: Insurance plans and PBMs stress the cost-saving justification. From their viewpoint, tiering and utilization management prevent waste and keep premiums lower. For instance, by law Medicare Part D plans must demonstrate that placing a generic in a lower tier significantly saves money; plans often show that generics cost less even after accounting for co-pay differences ([1]). By negotiating rebates, insurers can hold down formulary placement of preferred brands and direct patients to those drugs. Step therapy is billed as a way to enforce evidence-based medicine: patterns of care often have one or two first-line drugs proven in guidelines, and the insurer argues patients should reasonably try those before moving to experimental or second-line treatments. The Valeris pharmacy consultancy notes that tiering “determines how accessible a drug will be in the market, which directly influences how many patients can access the medication” ([2]). Thus, formulary design is touted as a legitimate tool for managing the panoply of new therapies launching each year.
In terms of evidence, payers point to the clear financial results: as the Motheral review shows, step therapy nearly always saves money ([6]). They also note that not all barriers are “hard stops”: for example, if a patient truly needs a second-step drug, the appeals process typically succeeds eventually. And they emphasize that insurers must balance budgets; the same costly biologic that helps one patient could, at full price, reduce coverage or increase premiums for hundreds of others. It is disingenuous to frame that as purely altruistic or evil – it is fundamentally a resource allocation problem.
Industry also stresses ongoing improvements: many plans have implemented “gold card” programs that exempt certain high-performing physicians from prior authorization requirements due to their good track record. Insurers also monitor outcomes and adjust protocols: if a step requirement is causing excess harm (or if a new generic comes out), they will revise the rule. Regulatorily, they argue, step therapy and PA are allowed tools that have proven their worth in negotiation. They largely support recent pledges (e.g. the Aetna/Cigna initiative ([23])) to modernize PA and are open to standardizing forms (some even contributed to CMS’s electronic PA pilots).
Policymaker/Advocate Perspective: Legislators and regulators occupy a middle ground. They recognize that utilization management is here to stay, but they aim to impose guardrails. Many state and federal rules now require timely reviews and exceptions. For example, Medicaid regulations typically mandate ultra-rapid approval for urgent medications and scheduling of standard PA within a few weeks. The federal government’s plan to standardize PA timelines (as part of price benchmarking and market competition initiatives) shows growing willingness to regulate PA. Policymakers often cite patient stories (sometimes even testifying in hearings) to justify legislative interventions. Oversight agencies (like the state insurance commissioners) have launched investigations into the prevalence of PA delays, just as they did for insurance claim denials.
At the same time, policymakers must also consider the budgetary angle. State Medicaid directors have sometimes resisted overly strict step-therapy bans, warning that biologic drug costs could swamp their budgets без mis poling. Federal Medicare, which cannot use Medicaid rate-limiters, sees step therapy as a tool to negotiate better deals (as evinced by lifting the ban for Part B drugs ([22])).
Real-World Examples: To bring these issues to life, consider a few illustrative cases:
-
Rheumatoid Arthritis Patient (2021 Cohort Study): A multi-center study (Wallace et al.) tracked 225 RA patients needing the infusion biologics rituximab or infliximab ([41]). 71% of these patients’ insurers required prior authorization. Those requiring PA waited a median of 31 days for the infusion, versus only 27 days for patients with no PA. More dramatically, patients whose PAs were initially denied (requiring appeals) waited 50 days on average – nearly 5 weeks – to start treatment ([41]). During these waits, 82% of patients with denied PAs needed rescue corticosteroids. This example illustrates how PA can convert a routine treatment plan into a multi-month ordeal, with added medication (and side effects) just to bridge the delay.
-
Psoriatic Arthritic Patient (Case Report, 2025): A patient with chronic psoriasis co-authored a letter describing her journey under step therapy ([20]). She initially achieved control on a biologic (a Tier 5 drug), but years later insurers mandated newer protocols. When she later developed psoriatic arthritis, the plan required her to first try methotrexate (a known step 1) and then an older anti-TNF drug before allowing her biologic again. She recounts painful disease flares and emotional distress during this forced trial-and-error. Interestingly, as soon as she appealed successfully, her access to the preferred biologic was restored; the intervening hardship was purely a consequence of the insurer’s step slate.
-
Atrial Fibrillation Array (DOAC Modeling): As noted, a decision-analytic model compared “restricted” access to DOACs (requiring step or PA) with “unrestricted” coverage in 1 million Medicare patients ([16]). The model found that restricting access led to hundreds of excess strokes, TIAs, and major bleeds annually (57 more strokes, 61 bleeds per million patients) and 452 more deaths, costing an extra $8.0 million in healthcare resources ([16]). Even a mere tier change (making apixaban harder to access) caused 330 more strokes/embolic events per million patients and $6.5 million extra costs ([16]). While models have assumptions, this study powerfully quantified how even modestly tougher coverage rules for life-saving drugs can yield net harm in an elderly population. It underscores the principle that higher copays or steps on a highly effective drug (with no perfect substitute) can ripple through morbidity statistics.
-
Medicare/Regulatory Trend: In 2018 CMS issued a fact sheet raising awareness that Medicare Advantage plans would from 2019 be allowed to use step therapy for Part B drugs (“physician-administered” therapies) ([11]). Historically CMS had blocked such policies for traditional Medicare, arguing that patients should not have to fail drug A to get drug B in urgent hospital-based care ([22]). This policy shift was framed as part of broader efforts to rein in drug spending. It serves as an example that utilization management strategies evolve with politics: as administrations come in, step therapy that was once unthinkable for certain benefits becomes permissible.
These cases illustrate the tangible consequences of formulary rules. At one extreme are hard policy outcomes (like lives affected by DOAC access). At the other are everyday frustrations (calling insurers, waiting weeks). The empirical evidence complements these narratives by showing that, on average, utilization tools work as intended (patients use cheaper drugs, plan spending drops), but they can also carry significant downsides.
Implications and Future Directions
Moving forward, the landscape of drug coverage management is changing but the core tensions remain the same: how to contain costs while ensuring timely, appropriate care. Several trends and reforms are worth noting:
-
Digital Transformation of PA: The industry is working toward electronic Prior Authorization (ePA) systems that integrate directly into prescribers’ electronic health records. The expectation, under CMS’s new interoperability rules, is that drugs (alongside radiology and other services) will see standardized ePA transactions by 2026. In practice, this means a doctor ordering a specialty drug could see real-time formulary checks and possibly automated decision-making flags. Some payers are also piloting AI review tools to quickly flag simple PA cases for instant approval. These IT advances could significantly reduce paperwork delays, addressing one of the most frequent complaints. However, they do not inherently change the underlying policy – a drug will still need authorization, albeit through a faster channel. The Axios report ([25]) suggests that patients on injectable or physician-administered drugs might not benefit as much from these rule changes in the near term, since the current focus has been on hospital-based care.
-
Legislative and Regulatory Reform: On the legal front, both step therapy and PA have attracted new laws. As of late 2025, over 38 states plus D.C. have step therapy laws, and most of these include protections for exceptions. Federal proposals have been floated in Congress to ban certain step-therapy maneuvers (e.g. Medicaid step therapy removal for certain classes like oncology) and to further streamline PAs. On the regulatory side, agencies are gradually tightening requirements. For example, some states now require formularies to justify tier placements (Kentucky, New Mexico) or to frequently publish formularies and exception data. There is also pressure from oversight bodies: if evidence shows that certain PA policies cause harm, regulators could mandate changes (e.g. mandating “gold carding” of high-volume docs or barring repeated denials).
-
Patient-Centered Innovations: Some plans are piloting “patient-friendly” formularies, such as value-based insurance designs (VBID) that reduce copays for high-value therapies. Under VBID, a Tier 3 drug might be dropped to Tier 1 for patients with specific conditions (to encourage adherence). While not yet widespread, these designs represent a counter-trend: rather than pushing patients down steps, they actively reduce financial steps in certain cases (for example, insulin often has virtually zero copay under new value arrangements). If expanded, VBID programs could help offset some negative effects of tiering. Similarly, “real-time prior authorization” programs have been introduced that promise insurance decisions within hours for routine drugs (though compliance and national availability remain limited).
-
Rise of Specialty/Tiers: The growing share of specialty medications (now over 50% of pharmacy spend in many plans) is likely to keep tier pressure high. We can expect more granular tiering (some plans already have 6+ tiers) and more “biologics vs biosimilars” choreography. As high-deductible health plans become more common (especially for younger people on employer coverage), tiering will be experienced differently: even a generic (Tier 1) can be unaffordable until meeting a deductible, so tier benefits might be muted at the point-of-sale.
-
Transparency and Appeals: In response to criticisms, many plans are improving transparency: publishing lists of step protocols and PA criteria, and fast-tracking some appeals. The US Office of Personnel Management (for federal employees) has even instituted a policy that if an expert panel of doctors disagrees with a PA denial, that opinion overrides the insurer. Patient advocates offer “decision trees” and hotlines to guide people through appeals. While incomplete, these efforts indicate an acknowledgment that patient outcomes must be better protected.
-
Unintended Consequences: We must also watch for game-playing. Insurers might respond to stricter PA rules by raising tier copays further (shifting the burden). Alternatively, PBMs and manufacturers might strike deals around step therapy (for example, by offering value-based pricing if patients reach certain outcomes). The evolving drug landscape (gene therapies, cell therapies) will challenge current PA models – a one-time curative therapy doesn’t fit neatly into a multi-step plan.
Conclusion. Drug formulary tiers, step therapy, and prior authorization are now integral tools of prescription benefit management. They arose to serve a necessary purpose – keeping drug spending from overwhelming insurers and entitlements – but they come with serious trade-offs in patient access and provider burden ([5]) ([18]). This report has reviewed the mechanics of each, examined evidence of their effects, and considered multiple perspectives and case examples. The overarching theme is that no policy comes for free: cost savings through higher tiers or utilization controls frequently results in delayed therapy or higher out-of-pocket costs. Stakeholders must therefore continually evaluate whether the clinical benefits achieved justify the administrative and patient burdens imposed.
Going forward, the challenge will be to refine these tools: to make tiering smarter (so needed drugs aren’t in inappropriate tiers), to make step therapy evidence-based and with quick exceptions, and to make prior authorization fast and predictable. Emerging solutions – digital PA systems, legislative guardrails, value-based copays – aim to thread that needle. The health care system must monitor outcomes closely and remain willing to adjust policies. Ultimately, these mechanisms should improve the value of drug spending (improving health per dollar spent), not merely reduce utilization. Ongoing research, regulatory oversight, and patient advocacy will shape the next generation of coverage rules, ideally ensuring that cost controls do not unduly sacrifice patient well-being.
References: The above analysis is grounded in official and scholarly sources. Key references include regulatory guidance (e.g. Medicare’s drug plan rules at [2†L47-L54]), industry analyses (Valeris [1†L15-L24]), peer-reviewed studies on formulary effects ([31]) ([6]), real-world cohort studies of PA delays ([41]), policy discussions (Henk et al. [9†L46-L54]), and recent news on legislative changes ([21]) ([19]). All claims and data above are provided with inline citations to the relevant sources.
External Sources (42)
DISCLAIMER
The information contained in this document is provided for educational and informational purposes only. We make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability, or availability of the information contained herein. Any reliance you place on such information is strictly at your own risk. In no event will IntuitionLabs.ai or its representatives be liable for any loss or damage including without limitation, indirect or consequential loss or damage, or any loss or damage whatsoever arising from the use of information presented in this document. This document may contain content generated with the assistance of artificial intelligence technologies. AI-generated content may contain errors, omissions, or inaccuracies. Readers are advised to independently verify any critical information before acting upon it. All product names, logos, brands, trademarks, and registered trademarks mentioned in this document are the property of their respective owners. All company, product, and service names used in this document are for identification purposes only. Use of these names, logos, trademarks, and brands does not imply endorsement by the respective trademark holders. IntuitionLabs.ai is an AI software development company specializing in helping life-science companies implement and leverage artificial intelligence solutions. Founded in 2023 by Adrien Laurent and based in San Jose, California. This document does not constitute professional or legal advice. For specific guidance related to your business needs, please consult with appropriate qualified professionals.
Related Articles
Patient Support Hub Programs: An End-to-End Guide
Learn about patient support hub programs in specialty pharma. This guide covers key workflows, technology, data management, and compliance for improving drug ac

Cohere Health: AI in Prior Authorization & Company Profile
Learn about Cohere Health, the health-tech firm using an AI platform to automate prior authorization. This profile covers its history, funding, and impact on UM
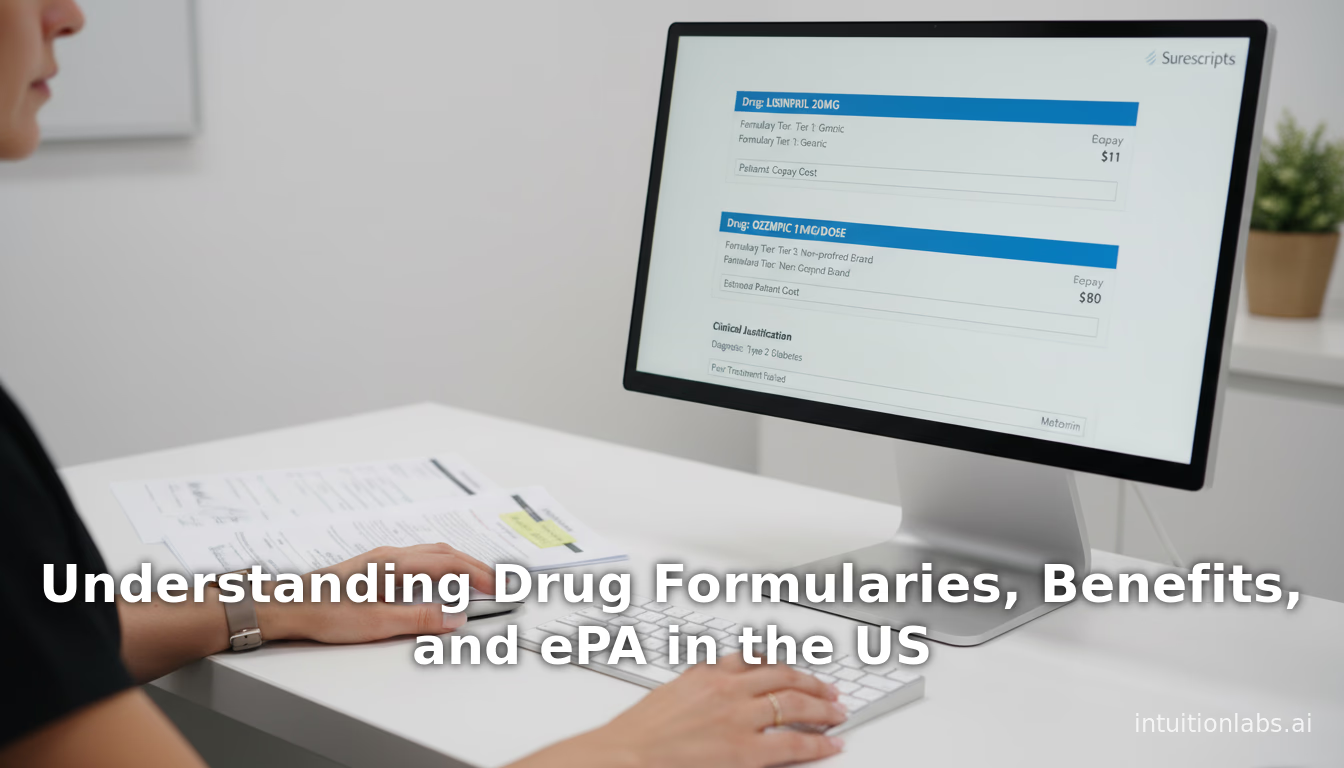
Understanding Drug Formularies, Benefits, and ePA in the US
An in-depth guide to US drug formularies, pharmacy benefits, and prior authorization (PA). Learn how P&T committees, tiers, and ePA systems work to manage costs