Most Expensive Drugs in the US: A 2025 Price List

The Most Expensive Drugs and Therapies in the USA (October 2025)
The United States now leads the world in record‐high drug prices, especially for one-time gene and cell therapies targeting rare diseases. A Reuters analysis found that median list prices for newly launched U.S. drugs more than doubled over four years (to about $300,000 in 2023) as treatments shifted toward orphan diseases ([1]) ([2]). In practice, that shift means single-dose cures are routinely hundreds of times more expensive than conventional drugs. For example, the newly approved gene therapy Lenmeldy (for metachromatic leukodystrophy) carries a list price of $4.25 million per dose ([3]) – the highest price of any U.S. medication to date. (Health economists at ICER noted that this one-time treatment might justify a cost up to ~$3.94 million based on its long-term benefits ([4]).) Other recent examples of “million-dollar” therapies include Bluembird’s Skysona ($3.0 M for X-linked adrenoleukodystrophy) ([5]) and Sarepta’s Elevidys ($3.2 M for Duchenne muscular dystrophy) ([6]). By comparison, traditional specialty drugs (like CAR-T cancer immunotherapies) typically run in the mid-$300,000s per course – still high, but well below these record-breaking therapies.
-
Lenmeldy (atidarsagene autotemcel) – A gene therapy for pediatric metachromatic leukodystrophy (MLD). Approved in 2024, Lenmeldy (from Orchard Therapeutics/Kyowa Kirin) is priced at about $4.25 million per patient ([3]). This therapy targets a deadly nervous-system disease affecting ~1 in 40,000 children; roughly half of late-infantile cases die within five years without treatment ([3]). The manufacturer is arranging outcome-based agreements with insurers, reflecting the drug’s enormous upfront cost and uncertain long-term outcome.
-
Elevidys (delandistrogene moxeparvovec) – A gene therapy by Sarepta for Duchenne muscular dystrophy (DMD). Alla 2023 FDA approval set its price at $3.2 million ([6]) for a single infusion. Elevidys is indicated for boys (age ≥4) with a common DMD gene mutation; it is projected to address about 90% of U.S. DMD patients (roughly 13,000 individuals) ([6]). Early sales data show rapid uptake (>$200 M in 2023), and analysts forecast over $1 billion in U.S. revenue by 2024 as coverage expands ([6]).
-
Hemgenix (etranacogene dezaparvovec) – A hemophilia B gene therapy by CSL Behring. FDA-approved in 2022, Hemgenix’s one-time infusion is priced at ~$3.5 million ([7]). It is designed to replace regular clotting-factor infusions by enabling patients to produce their own factor IX. At launch Hemgenix was billed as “the world’s most expensive therapy” ([7]), and its cost matches Pfizer’s later hemophilia B therapy below. (Both therapies achieved long-term remission in a majority of trial patients, but insurers and analysts continue to debate the value of the $3.5 M price tag.)
-
Beqvez (etranacogene dezaparvovec-drlb) – Pfizer’s hemophilia B gene therapy (new trade name as of 2024). Approved shortly after Hemgenix, Beqvez was launched at the same $3.5 million price point ([8]), eliminating bleeding in 60% of patients after one year versus 29% for standard care ([8]). The two therapies target the same disorder and hence represent fierce pricing competition: insurers typically will view them interchangeably.
-
Skysona (elivaldogene tavalent-l) – A Bluebird (now part of AbbVie) gene therapy for cerebral adrenoleukodystrophy (CALD), a fatal childhood leukodystrophy. Approved in 2022, Skysona costs about $3 million per treatment ([5]). It is indicated for boys (ages 3–12) with very early-stage X-ALD; as a one-time transplant of modified stem cells, it can halt disease in many patients. Because of reported long-term safety signals (cases of leukemia after treatment), the FDA now recommends evaluating alternatives first ([5]), but the price remains among the highest in the U.S.
-
Zynteglo (betibeglogene autotemcel) – A Bluebird Bio gene therapy for transfusion-dependent β-thalassemia. Approved in 2022, Zynteglo is priced at about $2.8 million ([9]) as a one-time procedure. It works by enabling patients’ bone marrow to produce normal hemoglobin, potentially freeing them from lifelong blood transfusions. Zynteglo’s launch price marked it as one of the most expensive U.S. drugs at the time ([9]), and it remains a benchmark for thalassemia treatment costs.
-
Zolgensma (onasemnogene abeparvovec-xioi) – Novartis’ gene therapy for spinal muscular atrophy (SMA). First approved in 2019 for infants, Zolgensma carries a list price of $2.125 million(over $2.1 million)per patient ([10]). This one-time IV gene replacement has been shown to dramatically improve outcomes in SMA Type 1, essentially curing many infants. At its launch, Zolgensma was the world’s most expensive drug ([10]), and while newer therapies have surpassed it, it remains an iconic example of the high-cost one-shot cure model.
-
Miplyffa (Hydroxypropyl beta-cyclodextrin) – A small-molecule therapy by Zevra Therapeutics for Niemann-Pick disease type C (NPC). Approved in 2024, Miplyffa is taken orally three times daily.The highest labeled dose costs about $106,000 per month, which extrapolates to ~$1.3 million per year ([11]). Even at that price, analysts expect insurers to secure substantial discounts (estimating a net price ~$600k/yr) due to the drug’s critical use in only ~900 U.S. patients ([11]).
Other high-cost therapies: Besides single-dose cures, some multi-dose regimens are also among the most expensive. For context, Spark Therapeutics’ Luxturna (for inherited retinal degeneration) costs ~$850,000 for the two-eye treatment (about $425,000 per eye). Biogen’s spinal muscular atrophy drug Spinraza (three initial doses plus annual maintenance) costs about $750,000 in the first year. Novartis’s CAR-T therapy Kymriah (for acute lymphoblastic leukemia) and Gilead’s Yescarta (for lymphoma) are roughly $475,000 and $373,000 per infusion, respectively. These are high by traditional standards, but still well below the multi-million-dollar therapies above.
Policy Context and Outlook
These sky-high prices have drawn intense scrutiny. U.S. prescription drug prices are far higher than in other countries, and politicians on both sides of the aisle have criticized the trend. President Biden’s 2022 Inflation Reduction Act empowered Medicare to negotiate prices for certain expensive drugs, though this mostly targets older blockbusters. By late 2025, the Trump administration also took steps: for example, in September 2025 President Trump announced a deal with Pfizer requiring Medicaid prices for Pfizer drugs to match prices in other developed nations ([12]). Meanwhile, industry analysts note that new drug launches increasingly target narrow patient populations, which justifies high prices in company view but raises fairness questions ([2]).
Indeed, a 2025 Reuters investigation reported that the median launch price for a new U.S. drug had reached $300,000 (a 35% jump from 2022), driven by rare-disease treatments ([1]). That same analysis highlighted a handful of extreme cases – for example, Niemann-Pick drug Miplyffa exceeds $1M annually and Lenmeldy costs $4.25M in a single dose ([2]). Policymakers and patient advocates emphasize that prices of this magnitude are unsustainable. Some proposals have emerged, including more aggressive price negotiation or linking prices to international benchmarks. (Notably, President Trump has publicly urged aligning U.S. drug prices with other countries’ levels ([13]).)
At the same time, manufacturers argue that these therapies, though costly, may deliver long-term value by reducing future care costs and improving patient lives. For instance, without treatment, many of these rare diseases are rapidly fatal or cause lifelong disability, which itself incurs high healthcare and societal costs. Outcome-based insurance deals are being explored: if a therapy fails, the manufacturer refund provision could mitigate financial risk. Nevertheless, the era of multi-million-dollar drugs has raised urgent questions about who will pay and how the system will cope with success in curing (rather than treating) rare diseases.
In summary, as of October 2025 the U.S. market’s priciest therapies are predominantly one-time gene or cell treatments for rare disorders, with list prices ranging from roughly $2 million up to $4.25 million per patient ([3]) ([6]). Other high-cost drugs (whether administered once or over time) tend to stay below the million-dollar threshold. This cohort of blockbuster orphan therapies sits at the frontier of medicine – and cost – with broad implications for healthcare budgeting and insurance design. Stakeholders continue to watch closely as new therapies enter the market and as policy efforts aim to rein in costs while rewarding medical innovation.
Sources: Authoritative news reports and analyses, including Reuters and healthcare industry outlets, were used to identify current highest-priced U.S. drugs and therapies ([3]) ([7]) ([5]) ([9]) ([10]) ([6]) ([2]) ([12]) ([11]). These sources provide launch prices, drug descriptions, and context for pricing trends.
External Sources (13)

Need Expert Guidance on This Topic?
Let's discuss how IntuitionLabs can help you navigate the challenges covered in this article.
I'm Adrien Laurent, Founder & CEO of IntuitionLabs. With 25+ years of experience in enterprise software development, I specialize in creating custom AI solutions for the pharmaceutical and life science industries.
DISCLAIMER
The information contained in this document is provided for educational and informational purposes only. We make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability, or availability of the information contained herein. Any reliance you place on such information is strictly at your own risk. In no event will IntuitionLabs.ai or its representatives be liable for any loss or damage including without limitation, indirect or consequential loss or damage, or any loss or damage whatsoever arising from the use of information presented in this document. This document may contain content generated with the assistance of artificial intelligence technologies. AI-generated content may contain errors, omissions, or inaccuracies. Readers are advised to independently verify any critical information before acting upon it. All product names, logos, brands, trademarks, and registered trademarks mentioned in this document are the property of their respective owners. All company, product, and service names used in this document are for identification purposes only. Use of these names, logos, trademarks, and brands does not imply endorsement by the respective trademark holders. IntuitionLabs.ai is an AI software development company specializing in helping life-science companies implement and leverage artificial intelligence solutions. Founded in 2023 by Adrien Laurent and based in San Jose, California. This document does not constitute professional or legal advice. For specific guidance related to your business needs, please consult with appropriate qualified professionals.
Related Articles
Rare Diseases in 2025: Diagnosis, Treatment & Policy
Explore the 2025 rare disease landscape, affecting 300 million people globally. Learn about diagnostic challenges, orphan drug development, and future policy di

Top Biotech Startups 2026: An Analysis of Emerging Trends
An evidence-based analysis of 20 biotech startups poised for impact by 2026. Learn about key innovations in gene therapy, diagnostics, AI, and sustainability.
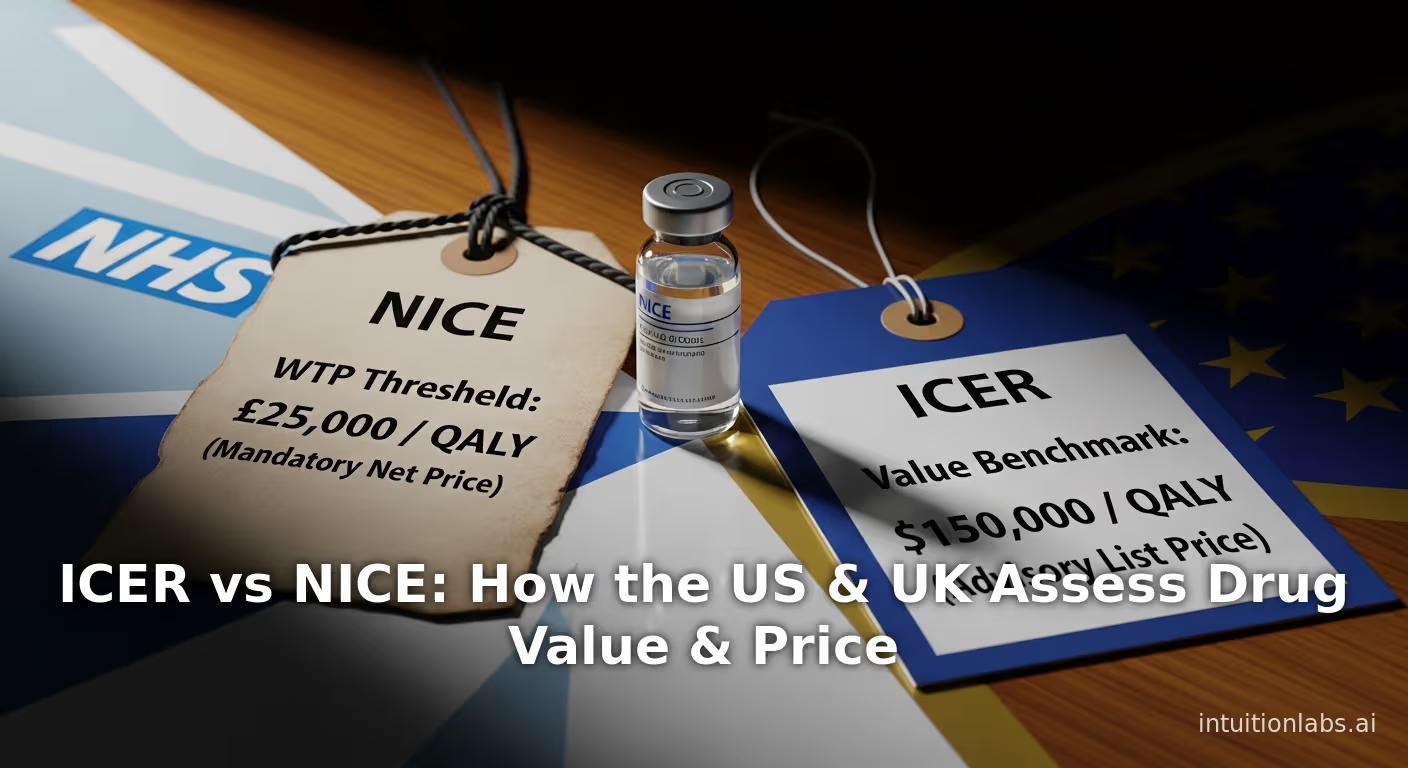
ICER vs NICE: How the US & UK Assess Drug Value & Price
An in-depth comparison of ICER (US) vs NICE (UK). Explore their methods, QALY thresholds, and how they assess drug value to influence global pricing floors.