Clinical Trial Phases 1–3: A Comprehensive Guide for Pharmaceutical IT Professionals
[Revised January 22, 2026]
Clinical Trial Phases 1-3: A Comprehensive Guide for Pharmaceutical IT Professionals
Introduction
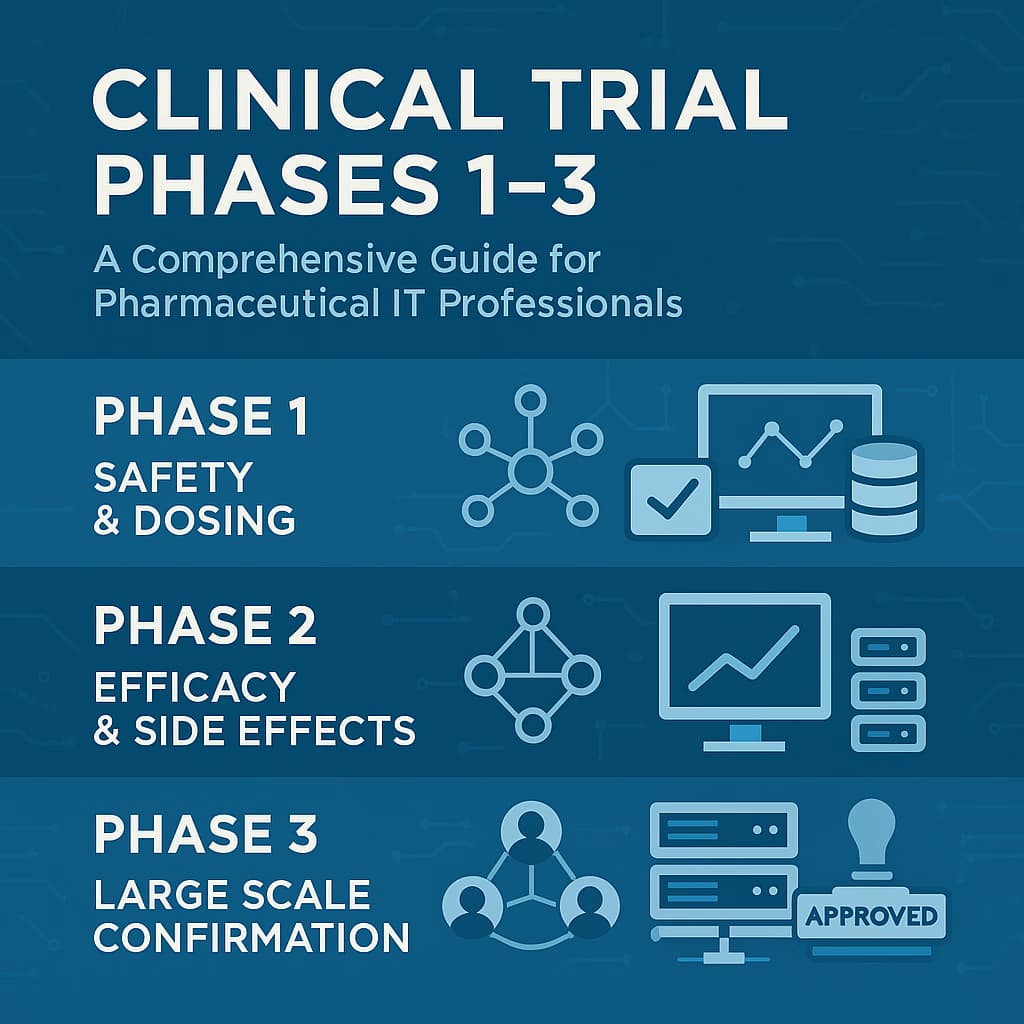
Clinical drug development proceeds through sequential Phase 1, 2, and 3 trials before regulatory approval. Phase 1 trials are first-in-human studies (often in healthy volunteers) focusing on safety and dosing. Phase 2 trials involve patients with the target disease to assess efficacy and optimal dose, while Phase 3 trials are large, confirmatory studies that establish clinical benefit and monitor adverse effects. Each phase has distinct objectives, design features, and regulatory requirements. Today's trials are heavily supported by information technology - from electronic data capture systems to clinical trial management software - so IT professionals must understand the clinical and regulatory context. Notably, ClinicalTrials.gov surpassed 500,000 registered studies in 2024, marking its 25th anniversary as the world's largest clinical trial registry, with approximately 22,000 new trials initiated annually.
All trials must operate under an active Investigational New Drug (IND) application (per 21 CFR 312) and comply with ethical and safety regulations (e.g. 21 CFR 50/56 for human subjects and ICH E6 Good Clinical Practice). FDA regulations mandate that sponsors submit essential preclinical and manufacturing data and a clinical protocol in the IND. Electronic systems (e.g. EDC databases) must also comply with 21 CFR Part 11 controls (validated systems, audit trails, secure user accounts). For example, FDA's Part 11 guidance emphasizes validation and audit trails for any e-records used to fulfill regulatory requirements. FDA's October 2024 guidance clarified that Part 11 is enforced once data enter the sponsor's EDC system (raw EHR data used as sources do not require Part 11 certification). A significant regulatory milestone is the finalization of ICH E6(R3) Good Clinical Practice guidelines on January 6, 2025, which modernizes GCP requirements to accommodate decentralized clinical trials, digital health technologies, and risk-based monitoring approaches. The FDA formally adopted E6(R3) in September 2025. Additionally, in early 2025 the FDA harmonized guidance on single Institutional Review Board (IRB) reviews for multicenter studies, streamlining the ethical review process. All phases require IRB review and informed consent, and serious adverse events must be reported under 21 CFR 312.32 and 312.64 to FDA and investigators.
Phase 1: Safety, Tolerability, and Dosage Finding
Phase 1 trials are first-in-human studies designed to evaluate a drug's safety profile, pharmacokinetics, and tolerable dose range. These studies enroll a small cohort (typically 20-100 subjects) and usually last several months. Most volunteers are healthy, though patient populations (e.g. oncology, HIV) may be used if the drug is expected to have unacceptable toxicity in healthy people. Common designs include single-ascending-dose (SAD) and multiple-ascending-dose (MAD) regimens, sometimes with sentinel dosing to mitigate risk. Investigators carefully monitor subjects for dose-limiting toxicities and measure drug absorption, metabolism, and excretion. If multiple doses or regimens are tested, crossover or parallel designs may be used with intensive pharmacokinetic (PK) sampling.
Key Phase 1 metrics include dose escalation rules (e.g. "3+3" design), cohorts of 3-6 per dose, and predefined stopping criteria. By the end of Phase 1, sponsors identify the maximum tolerated dose (MTD) and generate preliminary safety data to inform Phase 2. Recent industry data indicates that approximately 54% of investigational drugs proceed from Phase 1 to Phase 2, according to benchmarking studies from major pharmaceutical companies. Phase 1 trials are relatively short (often <1 year) and less expensive than later phases. A study of U.S. trials estimated Phase 1 costs at roughly $1.4-6.6 million (varying by complexity and therapeutic area). The typical sample size (20-100) and short duration contribute to lower overall cost and time for Phase 1.
FDA Guidance and Compliance - Phase 1. An approved IND (21 CFR 312.21) is required before human testing. FDA's Phase 1-specific guidance clarifies that Phase 1 IND submissions can be streamlined: sponsors may submit an integrated summary of animal toxicology data and minimal chemistry/manufacturing details, keeping the IND "no larger than two to three 3-ring binders ('jackets')". In practice, Phase 1 INDs focus on essential preclinical safety data and proposed protocols. Informed consent documents must clearly explain the experimental nature and risks. Institutional Review Boards (IRBs) must approve the protocol and safety monitoring plan. Although Phase 1 trials are small, all FDA regulations for human research apply: sponsors must comply with Good Clinical Practice (now ICH E6(R3) as of 2025) and report serious adverse events promptly (e.g. under 21 CFR 312.32). If a serious unexpected toxicity occurs, the IND may be placed on hold (21 CFR 312.42). Phase 1 also invokes 21 CFR 312.66 (IRB review) and Part 11 for any electronic records submitted.
IT Implications - Phase 1. Even small early-phase trials require validated IT systems. Electronic data capture (EDC) systems or eCRFs ensure reliable recording of safety labs and PK concentrations. Since data volume is low, sponsors may permit investigational sites to enter data directly into an EDC or use secure spreadsheets that later upload to a database. Nevertheless, all systems must be validated and secured: for example, Part 11 requires audit trails on eCRF fields and user authentication. IT personnel should integrate clinical labs via LIS (Laboratory Information Systems) interfaces to reduce transcription errors. Because Phase 1 often involves intense safety monitoring, some sponsors use electronic source (eSource) capture to directly log vital signs and ECG results. FDA's eSource guidance encourages capturing data electronically at the source and tracing it through to submission, which can reduce errors. In 2024, Medidata announced Rave Lite, specifically designed for Phase I and Phase IV studies with streamlined EDC capabilities. In short, Phase 1 IT work focuses on reliable PK/PD data collection and ensuring traceability of safety data (including metadata and time stamps), all under rigorous quality controls.
Phase 2: Efficacy and Dose Optimization
Phase 2 trials expand evaluation to patients with the target disease, to explore efficacy, optimal dosing, and continued safety. These trials typically enroll ~100-300 patients and last from several months up to about two years. A Phase 2 protocol often tests multiple dose levels (dose-ranging studies) or compares drug vs. placebo/active control, using endpoints that suggest therapeutic effect (e.g. tumor response, biomarker changes, symptom scales). Phase 2 endpoints may be surrogate or intermediate measures, since pivotal outcomes may take longer to emerge. Statistically, Phase 2 trials are not usually powered for definitive proof of benefit, but to estimate effect size and refine protocols. The lowest success rates occur in Phase 2 research, where only approximately 31-34% of drugs proceed to Phase 3 due to difficulties in obtaining proof-of-concept data.
Phase 2 designs vary widely by indication. Some trials are single-arm (no control) to get early efficacy signals, while others are randomized, double-blind controlled studies. A Data Safety Monitoring Board (DSMB) often oversees larger Phase 2 trials to review ongoing safety. Endpoints and sample sizes are chosen to balance resource limits with the need to detect clinically meaningful effects. Average costs are higher than Phase 1 - on the order of $7.0-19.6 million per trial in the U.S. - reflecting more patients, longer duration, and complex endpoint assessments. Trial durations also tend to lengthen (e.g. 1-2 years) as sponsors gather enough events to gauge efficacy and continue safety monitoring.
FDA Guidance and Compliance - Phase 2. Like Phase 1, Phase 2 trials operate under the same IND. Sponsors must submit detailed protocols (21 CFR 312.23(a)(5)) and informed consent forms to the IND. Because Phase 2 often explores multiple doses, sponsors should justify dosing regimens with pharmacologic data. FDA often recommends an End-of-Phase 2 (EOP2) meeting: after initial Phase 2 results, the sponsor may request FDA guidance on Phase 3 design and confirmatory endpoints. (EOP2 meetings are not mandatory, but common practice.) Good Clinical Practice (ICH E6(R3)) applies fully in Phase 2, including rigorous site monitoring and source data verification. All safety events (serious adverse reactions) continue to be reported in IND safety reports per 21 CFR 312.32. Phase 2 trials must also adhere to 21 CFR 312.66 (IRB approval) and record retention rules (maintaining records for several years after marketing).
IT Implications - Phase 2. Phase 2 trials require robust data management infrastructure. Electronic Data Capture (EDC) systems are standard to collect case report form (CRF) data across multiple sites. Sponsors often integrate an Interactive Voice/Web Response System (IVRS/IWRS) for randomization and drug supply management, which ties into the clinical database. Because subjects have the target disease, data may come from multiple sources: lab values (LIS interfaces), imaging, patient-reported outcomes (ePRO apps), and specialized devices (e.g. continuous glucose monitors). IT teams must ensure all inputs flow securely into the trial database. The larger sample size also demands stronger data cleaning and monitoring: data managers generate queries when inconsistencies appear, and ensure timeliness of entry. Information security is critical, since patient records contain Protected Health Information (PHI); systems must use encryption, role-based access, and routine backups. Clinical trial management systems (CTMS) are also used to track site performance, enrollment rates, and monitoring visits in Phase 2. On the standards side, sponsors typically plan for data submission by tagging fields with controlled terminology (e.g. MedDRA for adverse events, WHO Drug Dictionary for treatments) and following CDISC standards. In fact, FDA encourages using CDISC SDTM/ADaM formats for any datasets submitted to FDA (Phase 2 data may be submitted with an NDA later).
Phase 3: Pivotal Efficacy and Safety Trials
Phase 3 trials are large, confirmatory studies designed to provide substantial evidence of a drug's effectiveness and safety in the intended population. These studies typically involve 300-3,000 subjects or more, and last 1-4 years. Phase 3 trials are often multicenter (sometimes international), randomized, double-blind, and include the final selected dosing regimen(s). The primary endpoints are clinically meaningful outcomes (e.g. survival, disease remission rates, prevention of events) defined in consultation with FDA. These trials collect comprehensive safety data - including rare or long-term adverse events that smaller trials cannot detect. Given their scale, Phase 3 trials are resource-intensive. An estimated cost range per Phase 3 trial in the U.S. is $11.5-52.9 million, varying by therapeutic area and complexity, with some complex trials exceeding $100 million.
The probability of moving from Phase 3 to approval is around 70% for those drugs that reach this stage, but more than 40% of Phase 3 studies do not result in applications filed with FDA. By this stage, nearly all Phase 3 trials are randomized controlled trials (often versus placebo or active comparator). Statistical rigor is highest in Phase 3: sample sizes are calculated to detect the expected effect with sufficient power, and endpoints must meet prespecified success criteria (typically two-sided alpha=0.05). Notably, the FDA announced in December 2025 plans to require just one pivotal clinical trial (instead of two) as the default for new product approvals, though two trials may still be required in some cases. Phase 3 data form the core of the New Drug Application (NDA) or Biologics License Application (BLA).
FDA Guidance and Compliance - Phase 3. Phase 3 trials must follow the FDA IND regulations and additional requirements for pivotal studies. This includes rigorous protocol adherence, predefined statistical analysis plans (ICH E9), and timely results reporting. Sponsors continue to submit IND safety reports and annual IND reports (21 CFR 312.33). Because Phase 3 is the last clinical stage, trial quality is paramount: many sponsors engage independent Data Monitoring Committees to periodically assess blinded data for safety. FDA's guidance on E6(R3) GCP underscores that Phase 3 protocols must fully protect subject welfare and data integrity. Once Phase 3 is complete, the sponsor compiles data (per 21 CFR 314.50) into an NDA, including clinical summaries and tabulated data. Notably, FDA now requires or strongly encourages submission of standardized electronic datasets (CDISC SDTM/ADaM) with the NDA.
IT Implications - Phase 3. Phase 3 trials pose major IT challenges due to their size and complexity. An enterprise-grade EDC platform is essential to aggregate thousands of patient records from dozens of sites. Clinical Data Management Systems (CDMS) enforce data validation rules and manage query workflows. Large trials also rely on a CTMS to coordinate activities (site initiation, monitoring, enrollment tracking, regulatory documents). IT must integrate multiple data streams: Laboratory data via bi-directional interfaces, imaging via DICOM transfers, electronic patient diaries or apps for outcomes, and possibly wearable sensors or digital biomarkers. Data volume and heterogeneity require robust database infrastructure (often cloud-based or in controlled data centers).
From a compliance perspective, Phase 3 demands strict system validation and security. Before trial launch, all computerized systems (EDC, eCOA apps, CTMS, eTMF) must be validated to ensure they function as intended. FDA inspections expect sponsors to provide an inventory of these systems and their validation documentation. Electronic Trial Master Files (eTMFs) now replace paper binders; IT must ensure trial documents (protocols, consents, monitoring reports) are stored with audit trails and backups. Importantly, FDA's recent guidance clarifies that during audits, sponsors must produce all records (including metadata like timestamps and change histories) to "reconstruct a clinical investigation". This means every eCRF entry, amendment, and query is part of the regulatory record.
Data standardization and interoperability become critical in Phase 3. Clinical databases are mapped to CDISC SDTM domains so that datasets can be submitted or analyzed efficiently. FDA's Study Data Technical Conformance Guide mandates CDISC SDTM for clinical data submissions. CDISC released updated controlled terminology files in September 2025, including approximately 662 new QRS terms and 648 new terms across various terminology files. CDISC is also developing a Unified Study Data Model (USDM) that aims to integrate SDTM and ADaM into a single logical framework. Interoperability also involves integrating the clinical data warehouse with biostatistical analysis tools (e.g. SAS, R). On the security side, Phase 3 systems must comply with HIPAA (for patient privacy) and may undergo SOC 2 audits by sponsors. Network security (VPNs, encryption) is enforced for any remote access (especially if monitors work off-site). Finally, as trials are often global, multinational data transfer protocols (e.g. EU GDPR considerations for EU sites) may be relevant; data from foreign sites to the U.S. must still meet FDA Part 11 standards once entered into the EDC.
Industry Benchmarks and Comparisons
Below is a summary table of key metrics for Phases 1-3. Data are based on U.S. trials and industry studies:
| Phase | Purpose | Participants | Duration | Advance Rate | Typical Cost (US) |
|---|---|---|---|---|---|
| Phase 1 | Safety, tolerability, PK/PD | 20-100 (mostly healthy) | Several months | ~54% proceed to Phase 2 | $1.4-6.6 M |
| Phase 2 | Efficacy signal, dose-finding | ~100-300 (patients) | ~6 mo-2 yr | ~31-34% proceed to Phase 3 | $7.0-19.6 M |
| Phase 3 | Confirm efficacy and monitor safety | 300-3,000 (patients) | 1-4 yr | ~70% achieve approval | $11.5-52.9 M |
Additional industry trends: Clinical trial timelines are long. One analysis found the average durations were ~2.3 years for Phase 1, 3.6 years for Phase 2, and 3.3 years for Phase 3. In total, it takes roughly a decade (~10.5 years) to move a drug from Phase 1 to FDA approval. Success rates vary significantly by therapeutic area: according to industry research, the likelihood of approval from Phase 1 ranges from only 5% for oncology therapies to 26% for hematology. Benchmarking studies of leading pharmaceutical companies have found an average likelihood of first approval rate of approximately 10-14% across all drugs entering Phase 1. These attrition rates underscore the importance of efficient trial conduct and the use of biomarkers - research indicates that selection biomarkers can increase the likelihood of approval from 8% to 25%.
IT Infrastructure and Data Management in Clinical Trials
Information technology is integral to modern clinical trials. Key areas where IT supports phases 1-3 include:
-
Electronic Data Capture (EDC) and eSource: Sponsors now almost universally use EDC systems to collect CRF data. FDA guidance encourages capturing data electronically at the source (eSource) to improve quality. IT teams implement validated EDC platforms (e.g. Medidata Rave, Oracle Clinical One, Veeva Vault EDC) with role-based access and audit trails. According to the 2025 ISR Benchmarking Report, Medidata Rave EDC was named the #1 preferred EDC system by independent sponsor evaluations. For example, an investigator may enter exam results directly into an eCRF tablet at the visit. The system timestamps entries and logs changes, ensuring data integrity per 21 CFR Part 11. EHR-to-EDC interfaces are also emerging: patient baseline data can be auto-transferred from hospital records (with appropriate consent) to reduce manual entry.
-
Clinical Trial Management Systems (CTMS): CTMS software helps manage study workflows - tracking site contracts, site selection, patient enrollment, and monitoring visits. IT configures CTMS to notify managers of slow-enrolling sites or impending regulatory deadlines. Integration between CTMS and EDC can provide real-time metrics (e.g. enrollment by arm) for project managers. Major platforms like Medidata, Veeva, and Oracle now offer unified clinical suites that integrate EDC, CTMS, and other modules.
-
Decentralized Clinical Trials (DCTs): The FDA finalized guidance on Conducting Clinical Trials with Decentralized Elements in 2024, with a Guidance Snapshot published in October 2025. DCTs allow trial activities to occur at locations other than traditional sites, including via telemedicine or in participants' homes. DCTs can reduce site-related costs by 15-25% while potentially accelerating recruitment by 20-30%. Virtual visits cost approximately $200-$300 compared to $500-$800 for in-person visits. IT must ensure proper coordination of decentralized activities and account for data from a variety of inputs while maintaining 21 CFR Part 11 compliance.
-
Data Monitoring and Remote Access: Technology enables risk-based monitoring. Instead of 100% source-data verification on site, monitors use EDC dashboards and central statistical checks to find outliers or data anomalies. FDA's guidance notes that validated electronic records (with audit trails) allow remote monitoring: inspectors require that sponsors have documented all systems used and their validation status. Remote site monitoring using VPN access to EDC and video conferencing, accelerated during the COVID-19 pandemic, has become standard practice and is now explicitly supported by ICH E6(R3).
-
Data Security and Compliance: All clinical trial data are sensitive PHI. IT must ensure encryption of data at rest and in transit, multi-factor authentication for users, and network firewalls. Systems must be validated per GxP standards, and periodic security audits (e.g. SOC 2) are prudent. FDA's final Part 11 guidance emphasizes that, for inspections, sponsors need to supply all data and metadata to reconstruct a trial. Thus, backup and disaster-recovery plans are mandatory: if a study database is electronic-only, robust backup ensures no data loss. Regulatory compliance also means retaining records: 21 CFR 312.57 requires sponsors to keep trial records for 2 years after marketing or 5 years after IND discontinuation. IT systems must support these retention periods with reliable archival.
-
Standards and Interoperability: Data standards streamline regulatory review. The FDA mandates the CDISC SDTM (clinical tabulation) and ADaM (analysis) standards for submitted clinical data. IT and biostatistics teams work together to map EDC data into SDTM domains. Metadata (Define-XML) and annotations must accompany datasets. The new CDISC Analysis Results Standard (ARS) v1.0, released in 2024, provides a schema for linking analysis results with ADaM inputs. Outside the regulatory domain, interoperability with healthcare data is evolving: HL7 FHIR standards are being explored for trial data exchange (e.g. patient eligibility queries), and some sponsors use common data models (OMOP, Sentinel) to link trial data with real-world evidence. Ensuring correct use of standards requires coordination among data managers, statisticians, and FDA liaisons.
-
Artificial Intelligence and Emerging Technologies: Modern trials increasingly use digital tools and AI. In January 2025, the FDA issued draft guidance titled "Considerations for the Use of Artificial Intelligence to Support Regulatory Decision-Making for Drug and Biological Products", establishing a 7-step credibility assessment framework for AI in drug development. CDER has seen a significant increase in drug application submissions using AI components, spanning nonclinical, clinical, postmarketing, and manufacturing phases. AI-enabled simulation tools allow teams to model trials end-to-end before the first site is activated, testing eligibility criteria and predicting enrollment curves. Electronic Consent (eConsent) platforms manage the informed consent process with multimedia content. Electronic patient-reported outcomes (ePRO) systems allow patients to submit symptoms or diaries via smartphones. Wearable sensors and home monitoring devices can feed data into EDC in real time. IT must vet these technologies for data accuracy and regulatory compliance. The FDA reports approximately 950 FDA-cleared AI/ML medical devices by mid-2024, with roughly 100 new approvals each year.
Conclusion
Phases 1-3 trials form the core of drug development, each with distinct goals, designs, and regulatory expectations. Phase 1 focuses on safety and dose; Phase 2 on preliminary efficacy; Phase 3 on confirmatory evidence for approval. Key industry benchmarks (such as sample sizes, durations, success rates, and costs) differ markedly by phase, and sponsors plan accordingly. The regulatory landscape has evolved significantly with the finalization of ICH E6(R3) in January 2025 and its FDA adoption in September 2025, modernizing GCP for decentralized trials and digital technologies. For IT professionals, supporting these trials means deploying robust, validated electronic systems for data capture, management, and analysis - all under strict FDA standards (21 CFR 312, Part 11, ICH E6(R3)). Familiarity with regulatory guidance (e.g. IND content, eSource, Part 11, and DCT guidances) is essential. In summary, effective IT infrastructure (EDC, CTMS, secure databases, adherence to data standards, and AI-ready systems) is critical to the success and compliance of clinical trials in the pharmaceutical industry.
Sources: Authoritative references include FDA guidance documents and websites, ICH guidelines, CDISC standards, industry analyses, and clinical trial databases as cited throughout this article.

Need Expert Guidance on This Topic?
Let's discuss how IntuitionLabs can help you navigate the challenges covered in this article.
I'm Adrien Laurent, Founder & CEO of IntuitionLabs. With 25+ years of experience in enterprise software development, I specialize in creating custom AI solutions for the pharmaceutical and life science industries.
DISCLAIMER
The information contained in this document is provided for educational and informational purposes only. We make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability, or availability of the information contained herein. Any reliance you place on such information is strictly at your own risk. In no event will IntuitionLabs.ai or its representatives be liable for any loss or damage including without limitation, indirect or consequential loss or damage, or any loss or damage whatsoever arising from the use of information presented in this document. This document may contain content generated with the assistance of artificial intelligence technologies. AI-generated content may contain errors, omissions, or inaccuracies. Readers are advised to independently verify any critical information before acting upon it. All product names, logos, brands, trademarks, and registered trademarks mentioned in this document are the property of their respective owners. All company, product, and service names used in this document are for identification purposes only. Use of these names, logos, trademarks, and brands does not imply endorsement by the respective trademark holders. IntuitionLabs.ai is an AI software development company specializing in helping life-science companies implement and leverage artificial intelligence solutions. Founded in 2023 by Adrien Laurent and based in San Jose, California. This document does not constitute professional or legal advice. For specific guidance related to your business needs, please consult with appropriate qualified professionals.
Related Articles

Clinical Trial Acronyms: A Guide to GCP, ICH, IRB & EDC
Learn about key clinical trial acronyms. This guide explains the definitions, history, and roles of GCP, ICH, IRB, EDC, and eTMF in clinical research.

GAMP 5 & CSA: A Practical Integration Guide for Pharma
Learn how to integrate GAMP 5 (2nd Ed.) and Computer Software Assurance (CSA). This guide details the shift from CSV to a modern, risk-based validation strategy
AI for IND & CTA Drafting: Benefits, Risks & Compliance Guide
Learn how generative AI and LLMs assist in drafting pharma IND & CTA submissions. This guide explains the benefits, risks, GxP compliance, and FDA/EMA guidance.