ENTER is an AI-first Revenue Cycle Management (RCM) platform designed to help healthcare providers reduce claim denials, eliminate administrative burdens, and get paid faster with unprecedented transparency. The platform replaces traditional billing modules and is EHR-agnostic, offering custom integration with nearly every major EMR, including eClinicalWorks and Allscripts. The core of the platform is built around proprietary AI modules:
- ClaimAI: Builds and scrubs claims using payer-specific logic, proprietary scrubbers, and real-time eligibility checks to achieve a high clean claim rate.
- PaymentAI: Automatically posts and reconciles payments 24/7, instantly converting EOBs to ERAs and comparing payments against contract values to identify underpayments.
- DenialAI: Leverages predictive analytics to spot issues before they trigger denials, and programmatically generates compliant appeals and reconsiderations with supporting documentation.
- ContractAI: Stores, manages, and analyzes every payer contract's fee schedule, supporting all contract types (fee for service, value-based care, etc.).
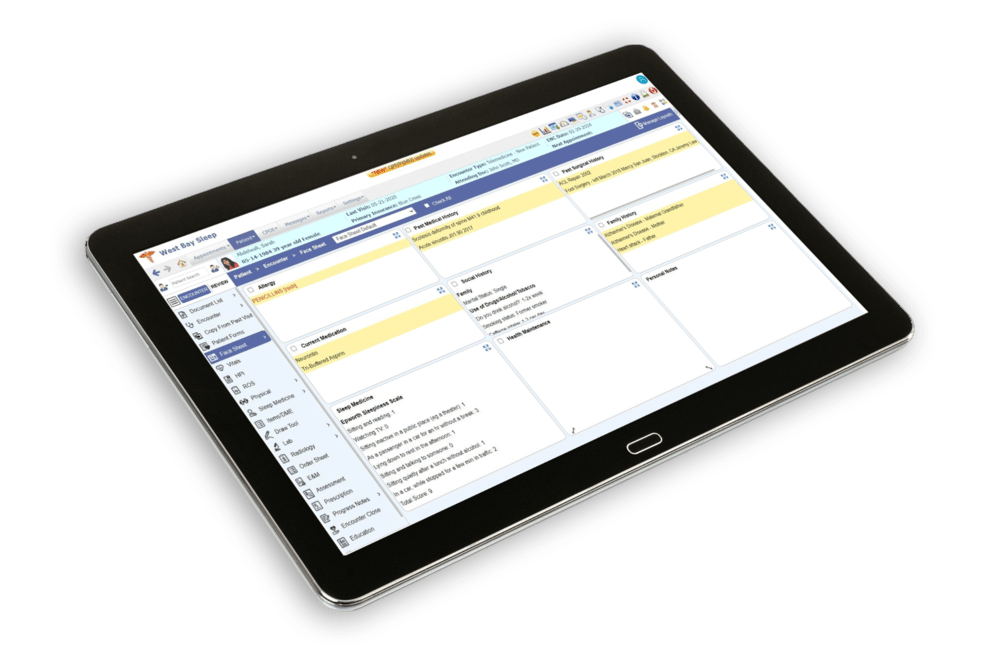
The solution is delivered as a cloud-based dashboard with a massive, state-of-the-art business intelligence platform for real-time reporting and self-service analytics. It is targeted at healthcare providers, from startups to large enterprises, including digital health providers and ambulatory practices. Implementation is rapid, typically taking 2-8 weeks.