AdvancedMD Claims Scrubbing, also known as Claim Inspector, is a proprietary, automated technology included as part of the AdvancedMD medical billing and Revenue Cycle Management (RCM) suite. It is designed to maximize revenue potential for independent medical practices by significantly reducing claim denials and accelerating reimbursement.
Product Overview and Key Benefits
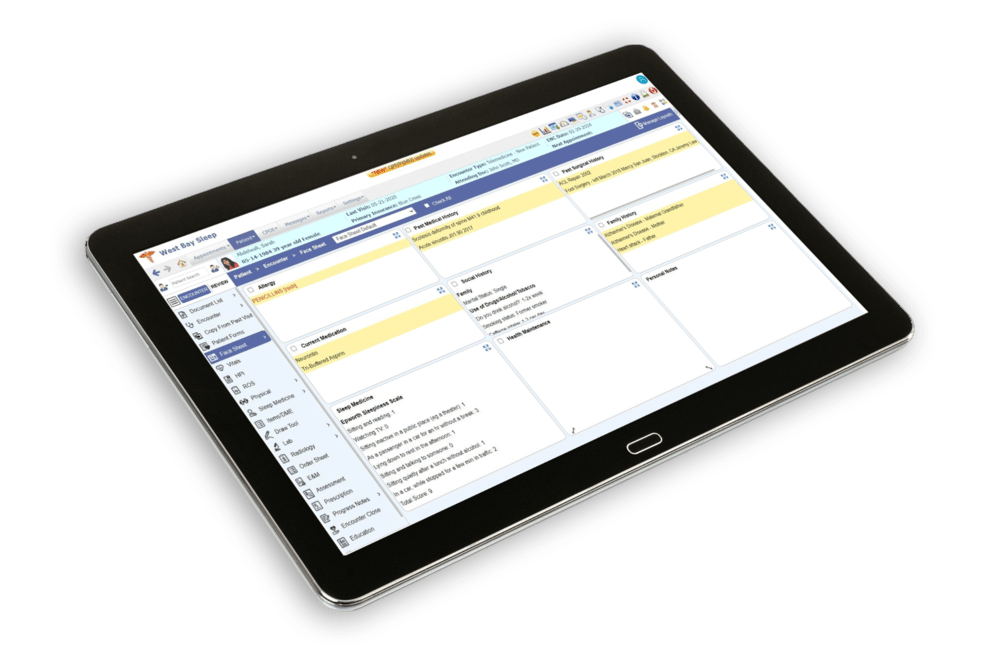
The Claims Scrubbing feature automatically reviews claims for millions of potential errors prior to submission to a clearinghouse. This proactive approach helps practices achieve a guaranteed minimum of 95% first-pass clean claim acceptance rate, which is a key metric for financial health. The tool is fully integrated within the cloud-based AdvancedMD Practice Management (PM) and Electronic Health Record (EHR) platform, ensuring a seamless and efficient workflow with no separate login required.
Main Features and Capabilities
- Automated Scrubbing (Claim Inspector): Automatically checks claims against a comprehensive knowledge base of over 119 million government and third-party industry edits, including CCI, HIPAA, and LCD errors.
- Prioritized Worklists: Automatically organizes unbilled claims and clearinghouse exclusions into prioritized worklists, allowing billing staff to quickly identify and correct missing or incorrect data (e.g., invalid diagnosis codes, incomplete facility addresses) before resubmission.
- Integrated Claim Submission: Facilitates electronic claim submission to over 1,800 payers through an integrated clearinghouse.
- Reporting & Analytics: Provides flexible reporting, audit logs, and run alerts to give visibility over claim status and problem payers, helping to shorten the payment cycle.
- Compliance Support: The scrubbing process is designed to support provider compliance by checking for coding and regulatory errors.
Target Users and Use Cases
The software is best suited for independent medical practices, medical groups, and large healthcare organizations (MSOs, IPAs, ACOs) that manage their own medical billing. It is a critical tool for RCM, used to reduce claim rejections, ensure accurate coding and billing, and accelerate cash flow.